If you’ve had a breast augmentation—or are thinking about getting one—you’ve probably heard the term capsular contracture come up in consultations or post-op care discussions. While this complication is relatively rare, it’s one of the most talked-about concerns among breast implant patients.
But what is capsular contracture exactly? Is it dangerous? How do you know if you have it? And what can be done if it develops?
In this guide, we’ll break down everything you need to know about capsular contracture, including the signs to watch for, how it’s measured (staged), what causes it, and how to treat or prevent it. Let’s dive in.
What Is Capsular Contracture?
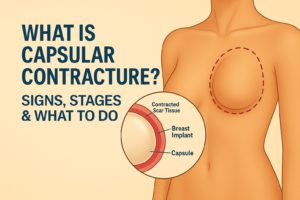
Capsular contracture is a condition that can occur after breast implant surgery when the scar tissue—or “capsule”—that naturally forms around the implant tightens or hardens excessively. This can cause the breast to feel firm, look distorted, or even become painful.
It’s important to understand that the formation of a capsule is completely normal. Any time a foreign object (like an implant) is placed in the body, the immune system forms a protective layer of fibrous tissue around it. This capsule helps “hold” the implant in place and is a natural part of healing.
However, in some cases, the capsule becomes too tight—compressing the implant and changing its shape, position, or softness. That’s what we call capsular contracture.
What Are the Signs of Capsular Contracture?
In the early stages, capsular contracture can be subtle. Some patients don’t realize anything is wrong until they begin noticing visible or tactile changes in how the breast looks and feels. Common signs include:F
- A breast that feels firmer or harder than usual
- One breast sitting higher or tighter than the other
- Roundness or distortion in the shape of the implant
- Tightness, discomfort, or aching in the chest
- Visible rippling or asymmetry compared to the opposite side
- In severe cases, pain or pulling sensations when moving the arm or chest
These symptoms can develop months or even years after surgery, though most cases appear within the first two years. If you notice any changes in the feel or appearance of your implants, it’s important to schedule a consultation.
The Baker Stages of Capsular Contracture
Plastic surgeons use the Baker Grading System to classify the severity of capsular contracture. This scale ranges from Grade I (normal) to Grade IV (severe). Understanding these stages helps determine whether intervention is needed.
Grade I (Normal): The breast is soft, natural-looking, and symmetrical. The capsule is present but not detectable by feel or appearance.
Grade II (Mild Contracture): The breast may feel a little firmer than normal, but the shape still looks natural. No visible distortion.
Grade III (Moderate Contracture): The breast appears noticeably firm and begins to show changes in shape or symmetry. The implant may look round, misshapen, or sit higher.
Grade IV (Severe Contracture): The breast is hard, visibly distorted, and often painful. The implant may feel tight or immobile, and daily movement or sleep may be uncomfortable.
Grades III and IV usually require medical intervention, while Grade II may be monitored depending on the severity and the patient’s concerns.
What Causes Capsular Contracture?
There’s no single cause for capsular contracture, but several factors are believed to increase the risk:
- Bacterial contamination during or after surgery (biofilm)
- Hematoma or seroma (blood or fluid build-up near the implant)
- Smoking, which impairs circulation and healing
- Autoimmune responses or strong immune system reactions
- Implant rupture or leakage
- Infection (even a minor one can trigger a response)
- Previous capsular contracture on the same or opposite side
While anyone with implants can technically develop it, choosing a skilled surgeon and following post-op instructions carefully can significantly reduce your risk.
How Is Capsular Contracture Treated?
Treatment depends on the severity of the contracture and how much it’s impacting your appearance, comfort, or quality of life. Options include:
1. Non-Surgical Management (Early Stages)
For mild cases (Baker Grade II), non-invasive methods may help slow progression:
- Massage or displacement exercises
- Ultrasound therapy or external compression
- Anti-inflammatory medications
- Leukotriene inhibitors like Singulair (sometimes used off-label)
These are typically more effective when started early and under surgeon supervision.
2. Surgical Correction
For moderate to severe cases (Grades III–IV), revision surgery is often recommended. Common options include:
- Capsulectomy – removal of the thickened scar capsule: Over time, a thickened layer of scar tissue—called a capsule—can form around your implants. In some cases, this capsule becomes hard, painful, or distorts the shape of the breast (a condition known as capsular contracture). A capsulectomy involves surgically removing the entire capsule surrounding the implant to eliminate tension, relieve discomfort, and create a healthier environment for a new implant (if placed). This technique is often used when the scar tissue is particularly dense or problematic.
- Capsulotomy – incision into the capsule to release tightness: If the capsule is less severe but still causing firmness or shape irregularities, your surgeon may perform a capsulotomy. This involves making small incisions in the capsule to release tightness and allow the implant to sit more comfortably and naturally. It’s a less aggressive approach than capsulectomy and is often used when reshaping or repositioning the implant rather than removing it entirely.
- Implant exchange – replacing old implants with new ones: Many revision procedures involve simply replacing old implants with new ones—especially if they’ve ruptured, rippled, shifted, or the patient desires a change in size, shape, or material (for example, switching from saline to silicone). Implant exchange can refresh your look and address aging implants without major reconstruction, particularly if there’s no significant capsular issue.
- Switching planes – moving the implant from above to below the muscle (or vice versa): In some cases, implants placed above the chest muscle (subglandular) or below it (submuscular) may no longer provide the best aesthetic result. Your surgeon may recommend switching the implant’s position—either from above to below the muscle, or vice versa—to improve contour, reduce visibility or rippling, and ensure better long-term support. This adjustment is often done in tandem with implant exchange or capsular work for optimal results.
- En bloc removal (for certain complex cases, especially with rupture or textured implants): En bloc capsulectomy is a more complex technique used in specific situations—most commonly when a patient has a ruptured implant, textured implants linked to health concerns, or requests full removal for peace of mind. The implant and its surrounding capsule are removed together in one piece, without opening the capsule inside the body. This approach can minimize contamination of surrounding tissues and is particularly important for patients concerned about BIA-ALCL or systemic symptoms potentially linked to their implants.
Our expert plastic surgeons tailor the approach based on your unique anatomy, the type of implant you have, and your aesthetic goals.
Aspen Therapy for Capsular Contracture: A Non-Surgical Alternative
While surgical revision remains the gold standard for moderate to severe capsular contracture, early-stage cases may benefit from a non-surgical solution like Aspen Ultrasound Therapy. This innovative approach uses a combination of therapeutic ultrasound waves, massage, and compression to soften the capsule and improve implant positioning—without going under the knife.
Aspen Therapy is FDA-approved and typically administered over a series of 10 sessions (usually 5 days a week for 2 weeks). It works by breaking down tight scar tissue, improving circulation, and restoring softness and symmetry to the breast.
When Is Aspen Therapy Recommended?
Aspen Therapy is best suited for:
- Grade I or II capsular contracture (early-stage firmness)
- Patients hoping to avoid revision surgery
- Post-operative patients showing early signs of tightness or asymmetry
- Those recovering from a capsulotomy or capsulectomy as a supportive treatment
In some cases, Aspen Therapy may also be used preventatively after implant placement to reduce the risk of capsule hardening during healing.
How Common Is Capsular Contracture?
Capsular contracture is one of the most common complications following breast implant surgery—and understanding the risks can help patients take proactive steps.
According to the American Society of Plastic Surgeons (ASPS):
- 75% of all capsular contractures occur within the first two years after implants are placed.
- Implants placed completely under the muscle have the lowest lifetime risk (4–8%)
- Partial submuscular placement carries an 8–12% lifetime risk
- Implants placed above the muscle (subglandular) have a 12–18% lifetime risk
Is Aspen Therapy Right for You?
If you’re experiencing early signs of firmness, discomfort, or asymmetry but want to avoid another surgery, Aspen Therapy could be a powerful, non-invasive option to restore a softer, more natural look and feel to your implants.
Your surgeon will evaluate your symptoms, implant history, and imaging (if needed) to determine if you’re a candidate for this ultrasound-based treatment—or if surgical revision is a better fit.
Can Capsular Contracture Come Back?
Unfortunately, yes—it can reoccur even after treatment. Patients who’ve had it once are at a higher risk of developing it again, especially without any change in implant type or placement.
That’s why during a revision, many patients choose to:
- Switch to smooth implants (less irritating than textured)
- Change the implant placement (from over to under the muscle)
- Add an acellular dermal matrix (ADM), such as Strattice or AlloDerm, to help reduce recurrence
Your surgeon will discuss all these options to help minimize your risk going forward.
Can You Prevent Capsular Contracture?
While it’s not 100% preventable, there are steps you can take to reduce your chances of developing capsular contracture:
- Choose a qualified, experienced plastic surgeon
- Follow all pre- and post-op instructions closely
- Avoid smoking before and after surgery
- Attend all follow-up appointments
- Monitor your implants regularly for any changes
- Consider ultrasound-guided fat transfer or implant placement, which offers added precision and reduces trauma
At the South Florida Center for Cosmetic Surgery, we use meticulous surgical techniques and strict sterilization protocols to lower the risk of complications. Our priority is your safety and long-term satisfaction.
When Should I Call My Surgeon?
If you notice sudden firmness, changes in breast shape, or discomfort—especially on one side—it’s always best to call your surgeon. Early intervention can make a big difference in how easy the condition is to manage.
Don’t wait for pain or major changes. The earlier you address it, the better your options.
Final Thoughts: Stay Informed and Empowered
Capsular contracture may sound intimidating, but with the right knowledge and a skilled surgical team, it’s a manageable condition. Whether you’re considering breast implants or have already had them placed, staying informed and proactive is your best defense.
If you’re experiencing symptoms or simply want a second opinion, we’re here to help. At the South Florida Center for Cosmetic Surgery, we offer compassionate care, personalized solutions, and long-lasting results—whether it’s your first surgery or a revision.




